Claims denials put a big dent into the budgets of healthcare providers – something many organizations can’t afford today given the current pandemic. In an environment where everyone must do more with less, reducing claim denials could release vital revenue and staff time to create breathing space for quality improvement.
The good news? About 90% of claims denials are preventable when healthcare providers automate revenue cycle functions. In fact, providers could gain an estimated $9.5 billion by automating the claims management processes.
Here are 5 ways for providers to proactively reduce claim denials.
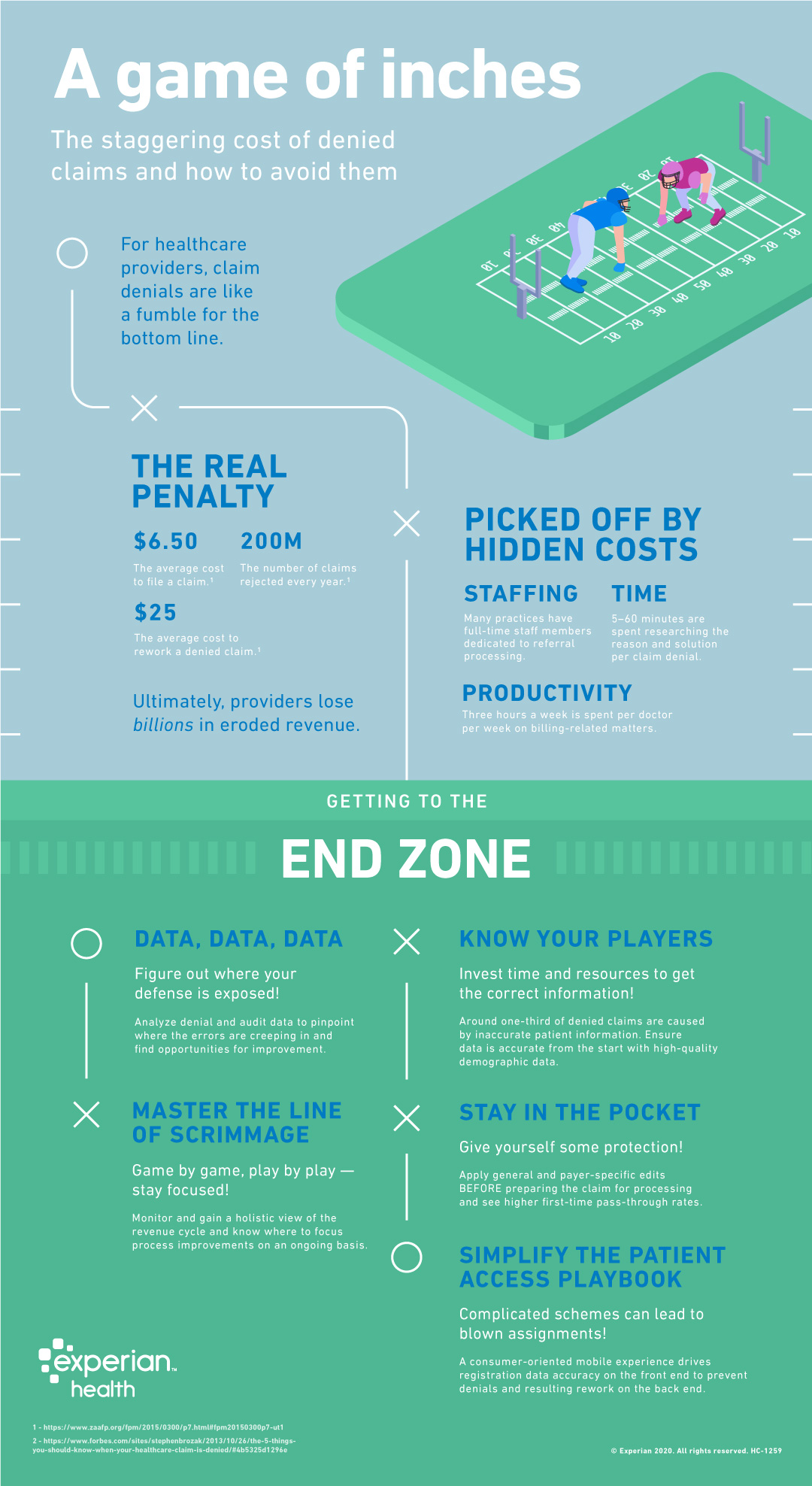
Healthcare providers should shift from reactive to proactive claim denial management, looking at the whole RCM process.
On the front-end, that includes streamlining the patient registration process. By achieving near-perfect levels of accuracy on the front-end, providers can prevent costly claims denials and unnecessary re-work on the back-end of the revenue cycle.
On the back-end, ideally, providers will use technology to prevent denials in the first place, improve processes for managing denials when they do occur, and then use a robust analytics platform to understand what went wrong so it can be avoided in future.



